Infestation of maggots
How to Kill Maggots | 5 Effective Solutions
How to kill maggots
Maggots can appear in many different areas throughout the home, yard, and — at worst — your pets. Each scenario will require a different treatment to rid you of the pesky invaders for good. Follow the guides below to learn how to kill maggots.
Locate all infested areas
As advised by Tonbridge and Malling Borough Council, locate all areas where maggots are feeding or living. Search through food products that are in especially dirty areas of the home. If the foundation of your home is rotting in any area, you could find maggots in different rooms of the house.
Killing maggots in the house
If you find maggots in the house, there are several ways you can kill them:
- Pour boiling water on any areas you suspect are infested.
- Thoroughly sprinkle the area with salt.
- Clean your trash bin with a mixture of water and lime, salt, or vinegar to prevent future infestations.
- Spray with an insecticide. If you find them in carpeting or baseboards in your home, you will generally need to spray.
- Use a spot spray treatment if the infestation is small, or use a broader spray to take care of a larger infestation.
Getting rid of maggots on pets
Before taking any treatment, you want to verify that your pets do have maggots. Look in recent wounds and between toe joints for anything moving or hard lumps under the skin.
If they’re found, the best thing that you can do to ensure the safety of your pet is to take them to the vet. Veterinarians will be able to kill maggots and rid your pet of the infestation without doing any harm to the animal.
Keep your pets clean and repel further infestations by washing them with pet shampoo during high season for egg-laying flies.
Spray or dust to clear maggots in the yard
First, you need to determine the scope of the maggot problem in your yard. Dig up the ground around plants that are suffering to check for any large holes dug into the root mass of the plants.
To clear out the infected area, use a vegetable and fruit spray all over the soil of the area. You can also dust the area with a similar treatment if there is a concern the spray could drift.
Killing maggots naturally
Maggots do not have a hard outer shell to protect them as other harmful insects do. This makes killing them by natural or organic means easier. Several home remedies are effective at ending a maggot infestation and cleaning out the infected areas.
If the maggots are in a trash bin, empty the trash bin and dispose of the materials that were inside. Then, fill the trash bin with boiling water. Another option is to set up a feast for the birds, putting out the trash can in an area where birds are common and can quickly pick through.
If you find areas infected with maggots outside of the bin, pouring lime or lemon juice over them should be enough to kill them. Make sure to spray it over the entirety of the area to kill any eggs that have not yet hatched. Another home remedy is to use diatomaceous earth, spreading it over the soil or infested area.
Another home remedy is to use diatomaceous earth, spreading it over the soil or infested area.
- Katchy Indoor Insect Trap: Use this product to repel flies (and other flying insects) as well as reduce odors.
- Harris Home Insect Killer: An insecticidal spray used to eliminate infestations.
- Medicated Shampoo for Dogs: Shampoo formulated by veterinarians to treat insect infestations in the coat and skin of dogs.
- Bonide Insect Control for Plants: Pest control to spray on vegetables and fruits as well as into yard and soil to kill harmful insects.
- Ortho Insect Kill: Kills insects on contact while staying active for up to eight months after soil application.
What do maggots look like?
Maggots are baby flies or the larval stage of a fly. They are conically shaped and often a grey or creamy white color. It is hard to differentiate the species of flies from their maggots, but if this is your goal, the University of Kentucky has put together a guide to recognizing larval types. Most maggots found in or around the home are from the common housefly or bluebottle fly.
Most maggots found in or around the home are from the common housefly or bluebottle fly.
Maggots are burrowers with their head-end being the more pointed end for digging in. Depending on the kind of fly, maggots feed on either live or rotting materials. They burrow in as they eat through the material, leaving circular, chewed holes scattered throughout.
If you’ve spotted these pests in your home, you’re probably wondering how to kill maggots, where they come from, and how to get rid of them for good. Here’s everything you need to know.
How do you get maggots?
The top causes of maggots in or around your home include improperly stored trash, excess dog feces, or the presence of an animal carcass. The female flies are attracted to such materials and lay their eggs on them. When the eggs hatch, the maggots burrow into the material and begin to eat until their next metamorphic stage.
Although they are quiet invaders, maggots should be dealt with quickly. Some of the dangers of maggots include fly infestations and animal sickness if you have pets. If they get into any food meant for human consumption, they can cause bacterial poisoning.
Some of the dangers of maggots include fly infestations and animal sickness if you have pets. If they get into any food meant for human consumption, they can cause bacterial poisoning.
How to check for maggots
In the home, maggots are generally easy to spot, with most of them being at least as big as a thumbnail. They will be crawling both in and out of any infested food substances. To check if they are inside of your garbage, take a stick or put on gloves to move the trash around and break food open to check inside.
To check if your pet has maggots, they will often be in a wound or under the skin. You can also check by feeling the area to see if there is a hard bump under the flesh of the wound.
Some maggots eat plant material. You may notice plants that were once healthy are dying without anything else changing in their environment. To check for maggots, you may need to pull up one of these plants and check for maggots in the root mass and in the plant’s hole.
Maggots will only feed for three to five days. The process from egg to fly takes anywhere from 14 to 36 days and, if the material is still in an edible state, the process may start all over again. If the material isn’t properly disposed of, then an infestation will only continue to get worse.
When to call a professional exterminator to treat maggots
The time might come when the maggot infestation is out of your control (or you just can’t stand to deal with it). This might be when the infestation has taken over several rooms in the house or if you have tried to clean an area out multiple times and the infestation has returned.
Another time that you may need to call a professional is if you are unable to identify the pest which will make it difficult to properly treat the problem.
How to keep maggots out of your home
To prevent a maggot infestation, it is important to prevent flies from being attracted to your home or yard. Be sure to clean up any food promptly and store it in sealed containers will keep odors from attracting flies into your home. If you have pet food out, you may want to keep the dish covered to keep flies out of it and remove old food quickly.
If you have pet food out, you may want to keep the dish covered to keep flies out of it and remove old food quickly.
If you keep compost in your yard, be sure to keep it covered or sealed to keep the flies out. Finally, make sure to keep the yard clean of any animal feces.
Starting with prevention will be an effective way to keep maggots out of the home. If you do suffer from an infestation, treating it with a chemical spray may be the quickest way to get rid of the problem. If you would prefer to use a home remedy, lime or lemon juice, salt, and boiling water are all useful methods to exterminate the problem.
Frequently asked questions
Q:
How do you get maggots in a home?
A:
Flies come in through open windows or doors if they sense any food or waste odors. They will lay eggs on the food and the eggs hatch into maggots.
Q:
Are there natural remedies to get rid of maggots?
A:
Using lime or lemon juice will kill maggots. Sprinkling a large amount of salt over them also does the trick. Strong vinegar or boiling water will kill them as well.
Sprinkling a large amount of salt over them also does the trick. Strong vinegar or boiling water will kill them as well.
Q:
What are maggots a sign of?
A:
Maggots may be a sign that food sat out for too long or was not disposed of properly, or perhaps you left windows or doors open for too long. Keep an eye on any pet wounds to prevent infestation there, too.
Q:
How do I get rid of maggots in my pets?
A:
You may need to shave the hair around their wound to effectively see and remove the maggots. Washing them with treated shampoo or applying a topical salve to the wound or infected area may also help, though the safest route is just to take them to the vet immediately.
Maggot Control: How to Get Rid of Maggots
This page is an expert guide on how to kill maggots using the products and methods suggested by our experienced pest control specialists. Follow this guide and use the recommended products and we guarantee you will be successful in getting rid of maggots.
Follow this guide and use the recommended products and we guarantee you will be successful in getting rid of maggots.
Maggots are a nightmare come true for almost everyone. They are filthy and slimy and not something you would ever want to see in your kitchen or anywhere else on your property. A maggot infestation can cause a lot of problems and you have to eliminate them entirely before they spread to other areas of the home.
If you've been scouring the internet looking for a solution to your home maggot infestation, our comprehensive guide below will lay out what maggots are, where do maggots come from, how to inspect for them, how to properly treat them and how you can prevent a maggot infestation from happening again.
Identification
The first thing that you should do before carrying out any pest control plan is to properly identify the pest you are dealing with and make sure they are maggots. Incorrect identification can lead to using the wrong treatment methods, wasting time and money. Below we will outline what maggots are, what they look like, and where maggots come from.
Below we will outline what maggots are, what they look like, and where maggots come from.
- Maggots are the larvae of flies. Around homes, maggots will most commonly be the larvae of either house flies or blow flies. The maggot larvae thrives in dirty and unsanitary conditions and can wreak havoc on anyone who ingests them through unhygienic food.
- When a fly lays eggs, they turn into maggots and hatch within a period of 7-20 hours. When the larvae hatches, maggots emerge, and they start to feed off anything that comes their way especially rotting and unsanitary things.
- Maggots look like tiny cream-colored worms and the largest can reach up to 20mm in length or 3/4th of an inch long.
- Maggots do not have any legs, but they do have two little hooks that serve as their mouthparts for feeding.
- Maggots and flies can become a problem any time of the year especially during the spring and summer when flies are more active.

- Maggots live for about 5 to 6 days in this phase before turning into pupae and eventually transitioning into adult flies.
Use the image and the description above to properly identify Maggots on your property. If you are not sure, contact us and our representative will assist you with the correct identification of your pest problem.
Inspection
Maggots don't just show up out of nowhere; they show up for a reason. Flies become attracted to some rotting material or spoiled food in your home and use that as a breeding ground to lay their eggs which hatch to become maggots. A detailed maggot inspection will help you pinpoint where the maggots are gathering and where you should focus your treatment.
Where To Inspect
Maggots are commonly found in areas where there is rotting food, organic material, or decaying matter and filth. In kitchens, they can be found in pantries in spoiled food, pet food, on rotting fruit or produce that has been laid out. Maggots can also be found in garbage cans that aren't sealed or the trash hasn't been tossed out for some time.
Maggots can also be found in garbage cans that aren't sealed or the trash hasn't been tossed out for some time.
What To Look For
You should look for maggots themselves or the appearance of adult flies. Maggots will appear in the form of small white worms in the house wiggling about in the food or filth they are found on. Flies will be hovering around filthy areas like garbage and feces and will breed and lay their eggs.
You should also look around your perimeter for entry points that flies could possibly use to gain access into your home (broken door and window seals, voids in the wall, cracks and crevices). Note these areas as they will be the areas where you will direct your treatment.
Treatment
Once you have confirmed maggot activity, it is time to begin treatment. Treatment will focus on getting rid of maggots along with getting rid of adult flies. Once you get control of flies, you will get control of maggots.
Before applying any of our recommended products you should first practice IPM (integrated pest management), which includes sanitation and modifications to your kitchen to discourage maggot activity.
Step 1: Sanitize Your Home
If you have found maggots around, it's likely you have found the source of why they are there. Decomposing food and filth are the main reasons you'd find maggot infestations in the home so you need to find that filth source and throw it out and then perform a thorough sanitation.
The main area to focus on is usually the kitchen since this is commonly where food can spoil and trash can pile up, which is where flies and maggots will gather. Clean your tabletops and counters, mop your floors, eliminate any moisture sources, toss out any old food and take out the trash. This is most important of all the steps because no amount of pesticide products will get the job done if your kitchen is not sanitized.
For maggots you have noticed in your garage or basement, sweep and mop the area well and remove any decaying filth and toss immediately in a sealed trash bin with a tight-fitting lid outside of the home. If the maggot problem is primarily outdoors, clean up the areas where you have seen flies such as around spoiled dog food, dropped food, pet feces and other such filth.
If the maggot problem is primarily outdoors, clean up the areas where you have seen flies such as around spoiled dog food, dropped food, pet feces and other such filth.
Step 2: Apply Flex 10-10 and Martin's IG Regulator
Once your home is sanitized, you should treat the maggots with a combination of a synthetic pyrethroid product called Flex 10-10 and Martin's IG Regulator. Flex 10-10 is a professional grade liquid insecticide labeled to treat flies and many more pests while Martin's IG Regulator is an insect growth regulator that disturbs the life cycle of flies and maggots by hindering the development of eggs, larvae and adults. This combination will kill maggots immediately and make it so flies can't reproduce.
Both Flex 10-10 and Martin's IG Regulator can be used indoors and outdoors and can be mixed together in a handpump sprayer for localized applications. For Flex 10-10, use 6.4 fl. oz. per 1 gallon of water. For Martin's IGR, use 1 oz. per gallon of water. A solution made with Flex 10-10 and Martin's IG Regulator can treat up to 1,500 sq. ft.
A solution made with Flex 10-10 and Martin's IG Regulator can treat up to 1,500 sq. ft.
To use a pump sprayer, fill the sprayer halfway with water and then add the appropriate amount of Flex 10-10 based on square footage of your treatment area. Fill with the remaining half gallon of water, close the sprayer lid and shake to mix the solution. Once well mixed, add the appropriate amount of Martin's IG Regulator and agitate once more. Pump your sprayer a few times to product a low-pressure spray and you are ready to apply.
- When spraying for maggots indoors, focus treatments around fly resting spots and entry points. This includes doors, windows, along windowsills and on surfaces around the trash can.
- For outdoor maggot control, spray ornamental plants, soil or mulchbeds where you have seen fly and/or maggot activity. You should also spray fly resting spots around doors, windows, trees and trashcans.
Step 3: Apply Pyrid Aerosol
To kill maggots or flies found in tighter spaces or structural voids, we recommend using Pyrid Aerosol. Pyrid is an pyrethrum insecticide that is labeled to kill flies and comes with a straw applicator tip for crack and crevice treatment. Pyrid does not have a residual and is used instead to directly spray pests, delivering a quick and lethal knockdown.
Pyrid is an pyrethrum insecticide that is labeled to kill flies and comes with a straw applicator tip for crack and crevice treatment. Pyrid does not have a residual and is used instead to directly spray pests, delivering a quick and lethal knockdown.
To use Pyrid Aerosol, attach the straw applicator tip to the Pyrid nozzle and apply to noted tight spaces and crevices. You could also use Pyrid Aerosol without the nozzle to treat open areas as a space spray such as above trash cans.
Step 4: Monitor Fly Activity with Professional 1x2 Fly Light Fly Trap
To monitor fly activity around the home to prevent them laying eggs and forming a new generation of maggots, install the Solutions Professional 1x2 Fly Light Fly Trap. When powered on, flies will be lured by the UV light from the trap and get stuck on the glueboards.
The Professional 1x2 Fly Light Trap is very easy to install. Mount the trap on a wall in an area of high fly activity such as a porch area, garage, or patio and plug it into an outlet and it will trap flies right away.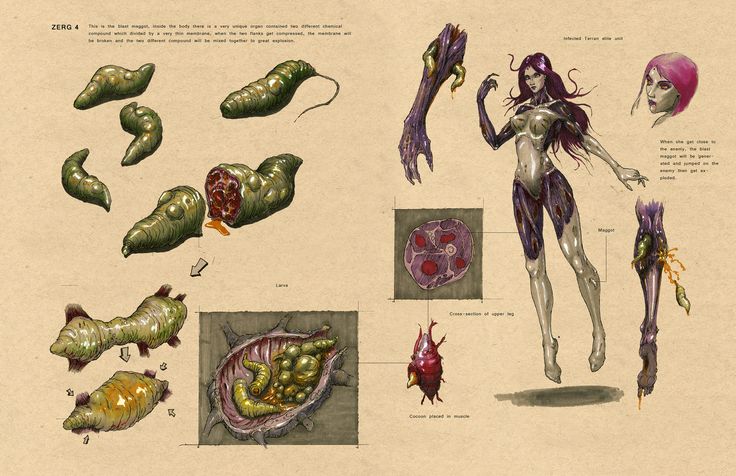
After you have treated and got rid of Maggots from your property, they may come back if you have not implemented preventative measures to keep them away. As we mentioned before, Maggots only appear when there are no proper hygiene standards maintained in an, be it at home in the kitchen, in a garage, a yard, or at a restaurant. Perform the following on a regular basis to prevent future encounters with Maggots.
-
Clean all your tabletops and kitchen counters.
-
Mop all the floors with an antibacterial cleaner.
-
Seal all your food in airtight containers.
-
Seal your garbage bags and cans properly to ensure nothing breeds or comes inside.
-
Seal all cracks and crevices with caulk to limit fly points of entry
-
Finally, make followup applications of Flex 10-10 monthly and Martin's IG Regulator every 6 months to keep Maggots and flies away all year round.

Key Takeaways
What are Maggots?
- Maggots are the larvae stage of flies and are cream-colored wiggly worms with an insatiable appetite.
- Maggots often invade kitchens and yards when there is rotting food or decomposing trash around. Flies view these areas as a perfect breeding ground to lay their eggs.
How To Get Rid of Maggots From Your Yard
- Remove or clean up the filth source in your yard to greatly reduce maggot and fly activity.
- Mix a combination of Flex 10-10 Insecticide and Martin's IG Regulator at a rate of 1 finished gallon per 1,500 sq. ft. to your yard to spray on flies and maggots.
- Spray ornamental plants, bushes, mulch beds, and anywhere else you have seen fly and/or maggot activity. You should also spray typical areas where flies land or where maggots are gathered such as around doors, fencing windows, trees and garbage cans.
How To Get Rid of Maggots In Your Home, Kitchen, Garage, etc.

- It is important to conduct a thorough cleanup of your home interior to remove the breeding source and discourage flies and maggots from arriving.
- Apply the Flex 10-10 and Martin's IG Regulator mixed solution in areas of your home to kill both fly maggots and flies, putting a halt to the infestation.
- Install the Professional 1x2 Fly Light Trap to lure and capture invading flies to stop their egg-laying.
- Use Pyrid Aerosol to directly kill spotted flies and maggots either in open areas or hiding in cracks and crevices.
Preventing Maggot Reinfestation
- Maintain a regular cleaning routine of your home and yard. Clean up and throw away rotting food, trash and pet feces.
- Seal as many entry points as possible with caulk to limit ways flies can get indoors to breed and lay maggot eggs.
- Make preventative applications of Flex 10-10 and Martin's IG Regulator at least every three months for continued protection against maggot infestations and fly invasions.

what it looks like, symptoms, signs and treatment
Olga Aksenova
3 018
Scabies is a parasitic skin disease caused by the scabies mite Sarcoptes scabiei.
CONTENTS
Scabies: definition of the disease
Ways of transmission of scabies
Types of scabies
Symptoms of scabies
Complications of scabies
Scabies in children
Diagnosis of scabies
Treatment of scabies
Prognosis and prevention
Sources
Scabies: definition of the disease
Scabies (scientifically known as scabies) is a common contagious skin disease.
In the last decade in Russia, the incidence of scabies has been officially kept at the level of 18-45 cases per 100 thousand people. But it can be much higher, since people do not go to the doctor: they try to cope with the disease on their own or are ashamed of their symptoms. nine0003
nine0003
The causative agent of scabies
The disease is caused by the scabies mite Sarcoptes scabiei, which feeds on flakes of dead skin. It spends most of its life in the skin, and appears on the surface only for mating.
The size of an adult tick is approximately 0.1 mm. The parasite has a powerful jaw, with the help of which it gnaws tunnels in the skin
As a rule, mating of ticks occurs in the evening. After it, the males die, and the females gnaw through human skin and make scabies in it, in which they lay 2-4 eggs. The hatched larvae come to the surface of the skin and penetrate into the hair follicles and flakes of the epidermis (upper layer of the skin). After a couple of days, they molt and become nymphs, and then they become adults, ready to mate. nine0003
Features of the scabies mite Sarcoptes scabiei:
- the mite quickly dies in the external environment: it is unable to absorb water from the air, therefore it dies from moisture deficiency;
- for the parasite, temperatures above 55 degrees are detrimental;
- adult females can penetrate the skin only in the most sensitive areas, and larvae - in any, due to their small size;
- is usually infected by females and larvae at the same time.
 nine0051
nine0051
Ways of transmission of scabies
There are two ways of transmission of scabies - direct and indirect.
Direct infection with scabies occurs during close bodily contact. There are known cases of tick transmission from an infected person to a healthy person even during a strong handshake.
Indirect infection with scabies occurs without direct contact with an infected person. This can happen in a bathhouse, a hotel, an entrance and in other places where many people touch the same objects on which ticks are located. nine0003
Scabies is usually contracted in orphanages, boarding schools, dormitories, barracks, prisons - wherever people live in large groups.
The risk of contracting scabies is higher in places where people work and live in tight communities.
When infested with larvae, the first symptoms may appear after 10-14 days - this is how long it takes for the mites to mature. And when infected by already fertilized females, there may not be an incubation period at all: the females will immediately begin to dig scabies and lay eggs in them in order to breed as soon as possible. nine0003
nine0003
Types of scabies
Typical scabies - the most common, accompanied by excruciating itching, scabies, nodules and blisters on the skin. The characteristic symptom of the disease - itching - usually appears 10-14 days after infection. Itching intensifies in the evening and at night, it is at this time that scabies mites are active.
Typical scabies is treated with scabicides, drugs that kill the mites and their larvae. The illness usually resolves within 2-3 weeks. nine0003
Clean scabies mostly occurs in people who shower or bathe in the evening. They have almost no nodules and blisters on their skin, strong scratching and bloody crusts.
Treatment for clean scabies is the same as for typical scabies. With the right choice of drugs and compliance with all the doctor's recommendations, recovery occurs in 2-3 weeks.
Norwegian (crustal) scabies is a rare and highly contagious form of the disease. It was first identified by Norwegian doctors in 1848 in patients with leprosy (leprosy). nine0003
It was first identified by Norwegian doctors in 1848 in patients with leprosy (leprosy). nine0003
As a rule, Norwegian scabies occurs in immunocompromised people, in patients with Down syndrome, HIV, dementia, oncological diseases, as well as in patients who take hormonal and cytotoxic drugs for a long time.
With Norwegian scabies, vesicles, nodules, cracks form on the skin, and then - rough crusts - gray-yellow or brown-black. Such crusts can, like a shell, cover large areas of the skin and prevent a person from moving normally. In the lower layers of the crusts, sinuous depressions are visible - scabies. When removing the crusts, extensive weeping erosions are exposed. Between the layers of crusts, a huge number of mites are found - up to 200 individuals in one square centimeter (for comparison: with typical scabies, there are usually no more than 10-15 of them). nine0003
Norwegian scabies can cause a micro-epidemic - when all family members, health workers and patients who are in the same room become infected with the disease.
The treatment of Norwegian scabies is long and takes place in two stages. First, the doctor removes the crusts from the patient's skin (sometimes local anesthesia is required), then prescribes anti-scabies, which will need to be used for a long time.
Scabies without burrows is less common than typical and is usually found in people who have been in contact with people with scabies. With such scabies, infection with scabies mite larvae occurs. Symptoms of the disease: single nodules and inflammatory vesicles on the skin. nine0003
Scabies without burrows usually resolves in 2 weeks, is treated in the same way as typical scabies - with anti-scabies drugs.
Scabious lymphoplasia - manifested by intensely itchy flat rounded bluish-purple nodules, which are most often localized on the trunk (buttocks, abdomen, in the axillary region), as well as on the elbows and genitals in men, mammary glands in women. The basis of the disease is the reaction of the body to the waste products of the tick. This happens in people who suffer from scabies for a long time. nine0003
This happens in people who suffer from scabies for a long time. nine0003
After full therapy, rashes may disappear in 2 weeks - 6 months.
Scabious erythroderma occurs in people who have been treated for a long time (up to 3 months) with typical scabies with corticosteroid ointments, antipruritic and sedative drugs. The disease is manifested by many itch moves that occur even in atypical places (between the shoulder blades, on the head, on the face). At the same time, itching is mild, and patients do not comb the skin, but rub it with their palms. nine0003
The treatment of scabious erythroderma is quite long - it may take up to 6 weeks until complete recovery.
Pseudosarcoptic mange is a type of scabies that affects dogs, pigs, horses, rabbits, wolves, foxes and other animals. Pseudosarcoptic mange can only be contracted from animals. It is not transmitted from person to person.
The incubation period is several hours. There are no scabies, since the mites do not breed on an unusual host and only partially burrow into the skin, causing itching. The rashes are concentrated on open areas of the skin and look like blisters, blisters, bloody crusts and scratches. nine0003
There are no scabies, since the mites do not breed on an unusual host and only partially burrow into the skin, causing itching. The rashes are concentrated on open areas of the skin and look like blisters, blisters, bloody crusts and scratches. nine0003
Pseudosarcoptic mange often resolves on its own after contact with the affected animal is stopped. If the symptoms recur or persist for several days, you should consult a doctor to make an accurate diagnosis.
Symptoms of scabies
The main symptom of scabies is unbearable itching, which intensifies in the evening and at night.
Itching runs along the burrows. They look like straight or curved lines that rise above the skin. The color of the lines can be dirty gray or whitish gray. Length - 5-7 mm. nine0003
Most often, burrows are found on the wrists, feet, male genital organs, in the interdigital spaces.
The skin of a person infected with scabies usually has blisters and nodules. In about a third of cases, young males and females of the parasite are found in them. You can see them with the naked eye: ticks look like white or yellowish dots the size of a poppy seed.
You can see them with the naked eye: ticks look like white or yellowish dots the size of a poppy seed.
Nodules with mites are located in the area of hair follicles. Bubbles are more often between the fingers, on the wrists. nine0003
The main symptom of scabies is excruciating itching
Complications of scabies
Complications of scabies in the form of dermatitis and secondary pyoderma occur in approximately 50% of patients.
Dermatitis - inflammation of the skin, which is manifested by redness, burning, tingling, itching, swelling of the affected area. Secondary pyoderma is a purulent-inflammatory skin disease caused by bacteria.
Less commonly, scabies develops microbial eczema - inflammation of the skin of an allergic nature caused by microbes.
Skin changes in scabies complicated by the addition of a secondary infection:
- staphylococcal impetigo - inflammation of the hair follicle caused by staphylococcus aureus;
- deep folliculitis - damage to the deep sections of the hair follicle, which leads to purulent inflammation;
- furunculosis - acute purulent-necrotic inflammation of the hair follicle, sebaceous gland and surrounding tissues; nine0051
- impetigo - vesicular-pustular rashes;
- paronychia - inflammation of the periungual fold.

Scabies in children
As a rule, children become infected with scabies in a direct way - through prolonged contact with the skin of an infected person. This happens when sleeping in the same bed, contact games, using shared toys. In addition, children can catch scabies in crowded groups - in orphanages, camps, hospitals, sports clubs, swimming pools. Teenagers are infected with scabies during sexual intercourse. nine0003
The course of scabies in children is usually more pronounced than in adults. Complications develop more often - microbial eczema, pyoderma (purulent-inflammatory skin lesions), impetigo (vesicle-pustular rashes), paronychia (inflammation of the periungual roller).
Symptoms of scabies in children:
- severe itching that worsens in the evening and at night;
- rash;
- scabies;
- nodules and vesicles on the skin.
Symptoms of scabies in children are usually worse than in adults
In infants and young children, rashes can be located on any area of the skin - including the face, scalp, palms and soles. The rash in babies often begins to get wet, there are multiple grouped vesicles in the lesions, scabious lymphoplasia of the skin.
The rash in babies often begins to get wet, there are multiple grouped vesicles in the lesions, scabious lymphoplasia of the skin.
In school-age children and adolescents, scabies affects the hands, feet, elbows, buttocks, genitals, intergluteal folds.
Diagnosis of scabies
The diagnosis of scabies is made by a doctor - a dermatologist, therapist or infectious disease specialist - on the basis of examination and patient complaints. nine0003
A clear sign of the disease is skin itching, which becomes unbearable in the evening and at night. Other symptoms that make it possible to suspect the disease are characteristic linear scratches and nodules on the skin.
Skin scrapings can confirm the diagnosis of scabies. However, it should be borne in mind that there may not be ticks in the biomaterial if the person has washed himself thoroughly before visiting the doctor.
Another way to detect a mite in a laboratory or clinic is to apply a drop of 40% lactic acid to the suspected itch, nodule, vesicle. Lactic acid loosens the epidermis well, and after a few minutes it can be carefully scraped off, placed on a glass slide and examined under a microscope. nine0003
Lactic acid loosens the epidermis well, and after a few minutes it can be carefully scraped off, placed on a glass slide and examined under a microscope. nine0003
The tick extraction method is also used. In this case, the doctor opens the blind end of the itch with a needle. The female is attached to the needle. Then the doctor takes the needle out of the itch along with the female and immerses it in a drop of water or 40% lactic acid. Then microscopy is performed.
Treatment of scabies
There are three ways to treat scabies: specific, prophylactic and trial.
Specific treatment is given to patients with symptoms of the disease and a clinically confirmed diagnosis. Scabicides are used - drugs that destroy the scabies mite and its larvae. nine0003
Prophylactic treatment is performed according to epidemiological indications - in scabies foci. However, people may not have symptoms.
Such treatment is indicated for everyone who has been in contact with an infected person: family members, sexual partners, nannies and nurses, members of close groups in orphanages, boarding schools, hostels, prisons, barracks.
Trial treatment is performed only in cases where the patient has symptoms of scabies, but the causative agent - scabies mite - is not detected. If after the use of anti-scabies drugs a positive effect occurs, then the diagnosis of "scabies" is considered confirmed. nine0003
Anti-scabies preparations
Ointments, emulsions, aerosols are used to kill scabies mites.
Basic scabicide preparations - scabicides:
- preparations containing esdepalletrin, a neurotoxic insect poison. Contraindicated in pregnant women, as well as in patients with bronchial asthma and obstructive bronchitis;
- benzyl benzoate (ointment, emulsion): 20% for adults and 10% for children from 3 to 7 years;
- sulfuric ointment 33%. The drug is contraindicated in children under 3 years of age. Has an unpleasant smell, stains clothes. Possible skin irritation, longer treatment; nine0051
- permethrin 5% (emulsion). The drug is not recommended for use in children under 1 year old, patients with liver and kidney diseases, lactating women;
- crotamiton 10% (cream, lotion).
 Pregnant women can use the medicine only according to strict indications. In addition, the drug is contraindicated in children under 12 years of age.
Pregnant women can use the medicine only according to strict indications. In addition, the drug is contraindicated in children under 12 years of age.
The doctor prescribes the dosage regimen. Self-medication can be hazardous to health.
General rules for the use of anti-scabies:
- apply medicines in the evening, with bare hands, not with a tissue or swab;
- carefully rub the preparations into the palms and soles;
- change underwear and bed linen after completion of the course;
- to treat simultaneously all those who are in the focus of infection.
The doctor may give the patient antihistamines or topical corticosteroids to relieve itching. Both of them are usually used in a short course. nine0003
If itching does not resolve within a week, it may be necessary to re-treat the skin with scabicide preparations after thoroughly washing the patient with soap and a washcloth.
Prognosis and prevention
With proper and timely treatment, the prognosis of scabies is favorable. The disease is cured in an average of 4-7 days, after which the doctor monitors the condition for 2-3 weeks. Residual itching may persist for another 10-14 days.
The disease is cured in an average of 4-7 days, after which the doctor monitors the condition for 2-3 weeks. Residual itching may persist for another 10-14 days.
Basic measures to prevent scabies:
- treatment and dispensary observation of all people with scabies;
- elimination of scabies foci: disinfection of bed and underwear;
- regular preventive examinations of children and adults in hospitals, nursing homes, colonies, orphanages, etc.
References
- Albanova V. I. Experience in the treatment of patients with scabies // Bulletin of Dermatology and Venereology, 1999. No. 2. P. 39–42.
- Malyarchuk A.P. Optimization of diagnosis, treatment and prevention of scabies: abstract of the thesis of a candidate of medical sciences. M., 2010.
- Malyarchuk A. P., Sokolova T. V., Lopatina Yu. V., Kiseleva A. V. Anti-scabies drugs: selection criteria // Clinical Dermatology, 2011. No. 9(2).
 pp. 53–59.
pp. 53–59.
Frequently asked questions
Scabies is transmitted during close bodily contact with an infected person or when sharing household items (this happens in nursing homes, orphanages, barracks, prisons - wherever people live in large groups). Cases of infection are known even with a firm handshake. nine0003
Scabies is highly contagious. The disease is transmitted by close physical contact or by sharing household items. That is why it is important for everyone who has been in contact with infected people to undergo preventive treatment.
For the treatment of scabies, special drugs are used - they destroy adult mites, their eggs and larvae. Antihistamines and corticosteroids may also be indicated to relieve itching.
Information checked
doctor-expert
Directory Diseases
Assess the article:
1
2
3
4
5
6
7
8
10
Useful article? Share on social networks:
IMPORTANT
The information in this section cannot serve as a sufficient basis for making a diagnosis or prescribing treatment. The decision on this should be made by the doctor on the basis of all the data available to him. nine0003
The decision on this should be made by the doctor on the basis of all the data available to him. nine0003
You may be interested
Peptic ulcer of the stomach and duodenum
Syphilis
Trichomoniasis
Ureaplasmosis
Gonorrhea (clap)
Gilbert's syndrome
Hereditary benign liver disease. It does not threaten life, but periodically causes unpleasant symptoms - yellowing of the whites of the eyes and skin and, less often, nausea, loss of appetite, and abdominal pain.
Anemia
A special condition in which the content of erythrocytes or hemoglobin in the blood is reduced, and all tissues of the body are deficient in oxygen.
A disease in which the lining of the small intestine is damaged when a person eats foods containing wheat and certain other cereals.
Most popular materials
Vitamin D Helicobacteriosis Yersiniosis Borreliosis - Lyme disease Calculous cholecystitis Order
studies
with departure
at home Use
bonuses
in the
loyalty program Get
consultation
specialist
online Subscribe
to Telegram -
channel
Hemotest Live
Top of page
Heartworm - Current guidelines for cats
Current guidelines for the diagnosis, prevention and treatment of heartworm in cats
last edited 03/16/2016
author Chernov V. N.
N.
Content
- Aspects of Morphology and Parasite Biology
- Cardiopulmonary form of dirofilariasis
- Pathogenesis and signs of disease
- Diagnostic approach
- Laboratory diagnostics
- Special studies
- Prophylaxis
- Treatment
- Cutaneous form of dirofilariasis
Introduction
The main material for creating the most reputable organizations to combat parasitic diseases of the animals, primarily the recommendations of the American and European companies for the combating of dirophylariosis, materials of European and American congresses devoted to dirofilariasis, the results of completed studies, articles by leading experts, to some extent, the opinion of a number of reputable practicing veterinarians and the experience of our clinic.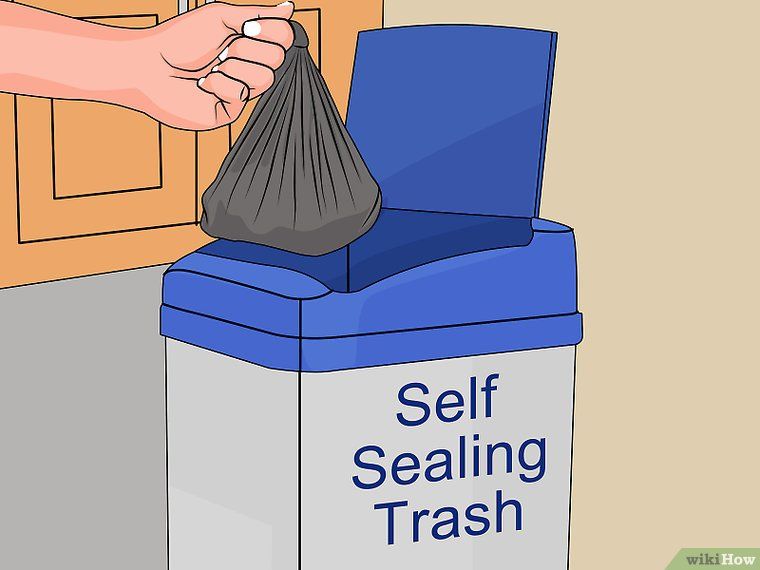 nine0003
nine0003
Aspects of morphology and biology of parasites
Dirofilariasis (Dirofilariasis, from the Latin "diro, filum" - "evil thread") is a helminthic disease caused by nematodes of the genus Dirofilaria. The length of adults reaches 40 cm, diameter up to 1.3 mm. The usual definitive host for dirofilaria are domestic dogs and other members of the canine family. The intermediate host is mosquitoes (genera Aedes, Culex, Anopheles). The total number of helminths that infect a dog varies from 1 to 250 individuals. In addition to dogs, other species can also be affected: wolves, foxes, coyotes, domestic and wild cats, ferrets, muskrats, sea lions, noses, as well as people. nine0003
In Ukraine and Russia, two varieties of dirofilaria are registered in cats:
— D. immitis — adults of this species parasitize in the pulmonary arteries and the right parts of the heart, causing a cardiopulmonary form of the disease;
- D.repens - adults of this species parasitize in the subcutaneous tissue and muscles, causing a skin form of the disease.
Cardiopulmonary heartworm disease
There are significant differences between heartworm disease in cats and dogs. Cats, although they are susceptible hosts, are more resistant to infestation. During a mosquito bite, infective L3 stage larvae enter the cat's body, develop in the subcutaneous tissue for several months, and then migrate into the systemic circulation and pulmonary arteries. Most of the helminths die when they reach the pulmonary arteries, this occurs 3-4 months after the onset of infection, at the stage of immature adults. In most cases of invasion, cats develop fewer than six adult helminths, usually one or two individuals. But, given the small weight of the cat, this is always a severe invasion. Approximately one third of the infected animals are observed infestation by same-sex individuals of helminths. nine0003
The duration of invasion is usually 2-3 years. More often than in dogs, atypical migration of helminths occurs (abdominal and pleural cavities, systemic arteries, central nervous system).
The prevalence of heartworm disease in cats is likely to be underestimated due to diagnostic limitations, a tendency to episodic manifestations of disease signs, and sudden death without confirmation of infection. It is believed that the prevalence of infection among domestic cats living in an endemic zone is from 5 to 15% of the total number of infected dogs. nine0003
Circulating microfilariae are rare, because invasion by same-sex individuals is common, the life span of microfilariae in the body of a cat is relatively short, there is an immune-mediated and drug-induced destruction of myrofilariae, as well as suppression of their production in adult female parasites.
Pathogenesis and signs of the disease
In all cases of infection in the lungs, similar histological changes develop, in addition to damage to the pulmonary arteries, bronchi, bronchioles and alveoli are always involved in the pathological process. Specific histological, radiographic changes, together with the characteristic clinical course of dirofilariasis in cats, are combined into a separate respiratory syndrome heartworm-associated respiratory disease (HARD). In some infected animals, despite the damage to the lungs, there are no symptoms of the disease throughout the entire period of invasion. If there are obvious signs of the disease, the symptoms develop in two stages: 1) the arrival of young dirofilaria in the pulmonary arteries, 2) the death of adult helminths.
In some infected animals, despite the damage to the lungs, there are no symptoms of the disease throughout the entire period of invasion. If there are obvious signs of the disease, the symptoms develop in two stages: 1) the arrival of young dirofilaria in the pulmonary arteries, 2) the death of adult helminths.
The first stage of the HARD syndrome develops 3-4 months after infection. The most typical symptoms are shortness of breath and cough. These early signs of the disease are the result of an acute vascular and parenchymal inflammatory reaction that occurs due to the arrival of immature helminths in the lungs and the subsequent death of most of them. A number of authors note that during this period, the disease can be misdiagnosed as “feline asthma”. In addition to a similar course of the disease, the symptoms, as in asthma, are easily stopped by corticosteroids. There may be vomiting, acute or chronic neurological disorders, sometimes anorexia, weight loss. In the presence of intermittent vomiting, not associated with food intake, in a cat living in an endemic zone, heartworm infection should be suspected. A number of other disorders such as ascites, hydrothorax, chylothorax, pneumothorax, ataxia, convulsions, syncope have been reported but are rare. nine0003
A number of other disorders such as ascites, hydrothorax, chylothorax, pneumothorax, ataxia, convulsions, syncope have been reported but are rare. nine0003
The second stage of the HARD syndrome is caused by the death of adult parasites. Decaying dirofilaria causes severe inflammation and thromboembolism in the lungs. In many cases, acute lung injury is due to an anaphylactic reaction that occurs in response to the death of an adult helminth. Acute severe respiratory failure, ataxia, collapse, convulsions, and hemoptysis often develop. The development of the second stage of the HARD syndrome often causes the sudden death of a cat. The average lifespan of symptomatic cats is about a year and a half (until one of the adult parasites dies naturally). nine0003
In all cases of infection in cats, proliferative changes in the intima of the pulmonary arteries develop, similar to arterial lesions in canine dirofilariasis. Clinically significant pulmonary hypertension is less common in cats because the number of adult helminths is small, the duration of invasion is relatively short, and the pulmonary artery involvement is usually localized. Accordingly, right ventricular heart failure is less common in cats than in dogs. Vena cava syndrome caused by dirofilariasis is also rare. The presence of even one or two helminths can lead to tricuspid insufficiency and murmur if the parasites are located in the right side of the heart. nine0003
Accordingly, right ventricular heart failure is less common in cats than in dogs. Vena cava syndrome caused by dirofilariasis is also rare. The presence of even one or two helminths can lead to tricuspid insufficiency and murmur if the parasites are located in the right side of the heart. nine0003
Diagnosis approach
Dirofilariasis in a cat is a diagnosis that is difficult to confirm, the most informative studies are: immunodiagnostic testing for D.immitis antigen, antibody test, radiography, echocardiography (ECHO). In many cases, studies are carried out repeatedly.
Laboratory diagnostics
Immunodiagnostic tests
As in dogs, single-use test systems are used for rapid diagnostics. The interpretation of antibody and antigen test results is complex, and in order to use them in a clinical setting, it is necessary to sufficiently understand what the diagnostic value is and what the limitations of these research methods are. nine0003
nine0003
Antigen testing
Antigen tests are highly specific, but have low sensitivity. The test systems detect a protein secreted by adult female dirofilariae, while in cats invasion is often found only in males, symptomatic invasion is often found, but with immature individuals. Tests are able to detect antigenemia after 5.5-8 months after the onset of infection. The study is not species-specific, i.e. test systems for dogs can also be used in cats. nine0003
If the test result is negative, it is considered that the probability of infection is not high. A positive result confirms the presence of adult helminths. Disadvantages of the test: immature helminths or males are practically not detected.
A recent study in cats showed that pre-heating the serum (103°C, for 10 min) before antigen testing can significantly reduce false negatives. To date, routine heat treatment of whey is not recommended, because. this is a violation of the instructions of the test manufacturers.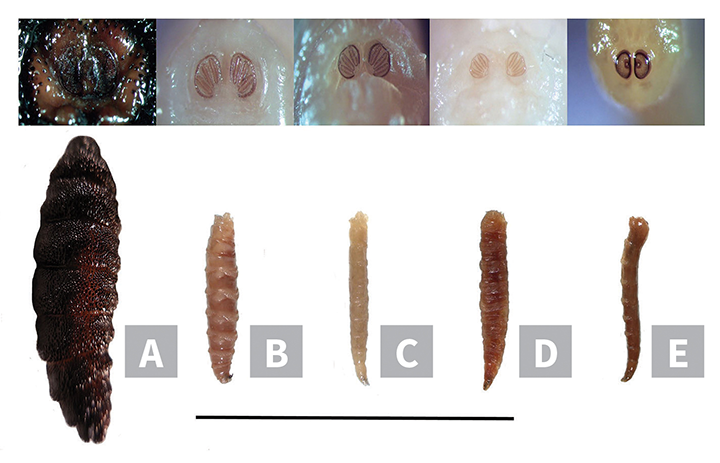 In such a situation, when the diagnosis of dirofilariasis is highly likely, but we do not have enough data to confirm it, it is advisable to repeat the antigen test, after thermally treating the serum. nine0003
In such a situation, when the diagnosis of dirofilariasis is highly likely, but we do not have enough data to confirm it, it is advisable to repeat the antigen test, after thermally treating the serum. nine0003
Antibody tests
The presence of antibodies produced in response to infection with Dirofilaria larvae can be detected as early as 8 weeks after infection. Tests detect invasion by both females and males. Testing, however, does not make it possible to judge whether adult helminths have developed and whether the animal is currently infested. A positive test result only indicates that an infection has occurred. To date, antibody tests are considered highly specific (98%), the sensitivity of tests based on the results of several studies is 32-89%. Tests from different manufacturers differ in their sensitivity to the detection of different stages of larval development. In some cases, if there is a positive antigen test, the antibody test may be negative. This is because antibody levels in cats decrease over time as adult helminths develop. Antibody testing is a species-specific test. nine0003
Antibody testing is a species-specific test. nine0003
If the antibody test is negative, infection is not likely; a positive result makes infection more likely. Disadvantages of the test: a positive result indicates larval infestation, but does not confirm adult development.
Microfilaria test
Most cats are amicrofilariaemic. Concentration methods of research (modified Knott method) are preferable to a native blood smear.
Special studies
X-ray
Regardless of the results of serological testing, characteristic changes on radiographs in cats living in an endemic area can be used to confirm the diagnosis. Radiography is necessary to assess the severity of the patient's condition, control the progression or regression of the disease. The most typical changes are an increase in the pattern of the pulmonary arteries of the caudal lobes (photo 1) and, especially, a local lesion of the peripheral pulmonary arteries. Unlike dogs, the characteristic radiographic picture of dirofilariasis in cats tends to normalize, over time, signs of invasion can completely disappear. In about half of affected cats, changes on radiographs are nonspecific. Often, symmetrical or asymmetric pulmonary inclusions of various sizes and densities are detected, without clear contours, sometimes - consolidation of the lobes of the lung, hydrothorax, pneumothorax, emphysema and flattening of the diaphragm. In some cases of infection, radiographs may remain normal. It should be noted that an increase in the bronchial pattern in a cat can also be a sign of dirofilariasis. nine0406 From Schafer M, Berry CR: Cardiac and pulmonary artery mensuration in feline heartworm disease. Vet Radiol Ultrasound 36:499, 1995. Severe disease in a cat with dirofilariasis, arrows indicate dilated, indurated, deformed pulmonary arteries. Photo 3 http://www.
Unlike dogs, the characteristic radiographic picture of dirofilariasis in cats tends to normalize, over time, signs of invasion can completely disappear. In about half of affected cats, changes on radiographs are nonspecific. Often, symmetrical or asymmetric pulmonary inclusions of various sizes and densities are detected, without clear contours, sometimes - consolidation of the lobes of the lung, hydrothorax, pneumothorax, emphysema and flattening of the diaphragm. In some cases of infection, radiographs may remain normal. It should be noted that an increase in the bronchial pattern in a cat can also be a sign of dirofilariasis. nine0406 From Schafer M, Berry CR: Cardiac and pulmonary artery mensuration in feline heartworm disease. Vet Radiol Ultrasound 36:499, 1995. Severe disease in a cat with dirofilariasis, arrows indicate dilated, indurated, deformed pulmonary arteries. Photo 3 http://www. petplace.com Angiogram of a cat with dirofilariasis.
petplace.com Angiogram of a cat with dirofilariasis.
Echocardiography
In some cases of invasion, echocardiography allows a definitive diagnosis, especially if the cat has several helminths. Pulmonary hypertension is less common than in dogs. Photo 4 Right parasternal approach along the short axis of the left ventricle at the level of the pulmonary artery. An adult dirofilaria is located in the right pulmonary artery. nine0406
Prophylaxis
In areas where drug prophylaxis for dirofilariasis in dogs is carried out, it is clearly necessary in cats. In one retrospective study, among the total number of cats infected with mature D. immitis, 25% were animals that were constantly indoors, their owners stated that the cats did not go outside.
Tab. 1 Dosage of macrolides for the prevention of heartworm disease in cats
Monthly use of one of the drugs shown in Table 1 is a safe and effective way to prevent the disease. The first treatment is carried out at the age of 8 weeks. In adult animals, in the absence of clinical suspicion of infection, testing for antigen and antibodies is not strictly required, but is recommended. Severe reactions to microfilarial extermination are not expected when macrolides are used in cats. Preventive treatments are recommended during the flight of mosquitoes and a month later, after the end of the flight. Start processing again a month before the start of the mosquito flight. Preferably, however, year-round prevention. nine0003
The first treatment is carried out at the age of 8 weeks. In adult animals, in the absence of clinical suspicion of infection, testing for antigen and antibodies is not strictly required, but is recommended. Severe reactions to microfilarial extermination are not expected when macrolides are used in cats. Preventive treatments are recommended during the flight of mosquitoes and a month later, after the end of the flight. Start processing again a month before the start of the mosquito flight. Preferably, however, year-round prevention. nine0003
Broadline combination preparation (fipronil, (S)-methoprene, eprinomectin, praziquantel) can also be used for drug prevention of heartworm disease in cats. ( Links to the results of studies of the drug)
Treatment
In animals with a confirmed or highly probable diagnosis, but the absence of clinical manifestations of dirofilariasis, it is recommended not to start treatment, but to monitor the patient's condition (repeat x-ray, antigen and antibody tests every 6 -12 months). This approach to patient management is based on the results of a study that showed that asymptomatic cats with invasion in 80% of cases spontaneously heal. nine0003
This approach to patient management is based on the results of a study that showed that asymptomatic cats with invasion in 80% of cases spontaneously heal. nine0003
In cases where infection is confirmed or highly likely and there are characteristic symptoms, corticosteroids are indicated. Empirical dosing regimen of prednisolone: 2 mg/kg/day, gradually lowering the dose over two weeks to 0.5 mg/kg every other day, and for two further weeks 0.5 mg/kg every other day. If symptoms recur, the course is repeated, the continuous use of corticosteroids is not recommended.
Adulticidal therapy with melarsomin is not recommended in cats. Melarsomin is considered the treatment of last choice for animals that are stable but show signs of disease that are not amenable to corticosteroids. nine0003
Aspirin and other NSAIDs do not improve prognosis and are thought to worsen prognosis.
Long-term use of macrolides at low doses, as in dogs, has adulticidal properties, reducing the number of adults. However, in cats, the problem is not only in the number of adult helminths, but also in a severe anaphylactic-type reaction that develops after their death. To date, there are no studies that show that macrolides increase the survival rate of cats with heartworm disease. The question of their use remains at the discretion of the doctor. nine0003
However, in cats, the problem is not only in the number of adult helminths, but also in a severe anaphylactic-type reaction that develops after their death. To date, there are no studies that show that macrolides increase the survival rate of cats with heartworm disease. The question of their use remains at the discretion of the doctor. nine0003
Animals with acute symptoms of PE and signs of shock receive appropriate supportive care (oxygen, corticosteroids, fluid resuscitation, bronchodilators). Aspirin and other NSAIDs are not indicated.
With sufficient experience and technical base, good results are obtained through surgical intervention. Extraction of helminths from the vena cava and the right atrium can be performed using flexible instruments to remove foreign bodies. Thoracotomy followed by ventriculotomy allows the extraction of helminths from the atria and pulmonary arteries using flexible instruments or even rigid alligator forceps. nine0003
In all cases of infection, regardless of the presence of symptoms and treatment tactics, repeat serological testing every 6-12 months.